Introduction
The Chinese University of Hong Kong (CUHK)'s Faculty of Medicine (CU Medicine) and the Prince of Wales Hospital (PWH), in collaboration with the Chinese Stroke Association (CSA) and the Beijing Tiantan Hospital (BTH), affiliated to Capital Medical University, have introduced the use of 0.23T low-field magnetic resonance imaging (lfMRI) technology in Hong Kong in August this year. This initiative marks Hong Kong's participation in a nationwide, multicentre clinical trial that incorporates the lfMRI technology into a new one-stop acute stroke management model called the Emergency Stroke Unit (ESU). The ESU model aims to enhance the efficiency and effectiveness of acute stroke diagnosis and treatment process.
The Global Burden of Stroke
Stroke is a leading cause of death and disability worldwide (Fig 1), affecting over 12.2 million individuals annually [1]. According to the World Stroke Organization, one in four people will experience a stroke during their lifetime. While stroke is often perceived as a disease of the elderly, 63% of strokes happened in people younger than 70 years old in 2019, indicating its broad demographic impact. The ageing global population, coupled with the prevalence of lifestyle-related risk factors, has led to a rapidly increasing stroke burden.
The economic cost of stroke is staggering. The total estimated worldwide cost of stroke (in international dollars) in 2017 was $451 billion [1]. Beyond the financial toll, strokes impose a heavy burden on patients, families, and healthcare systems. In many cases, stroke survivors face long-term disabilities that require intensive rehabilitation and caregiving support.
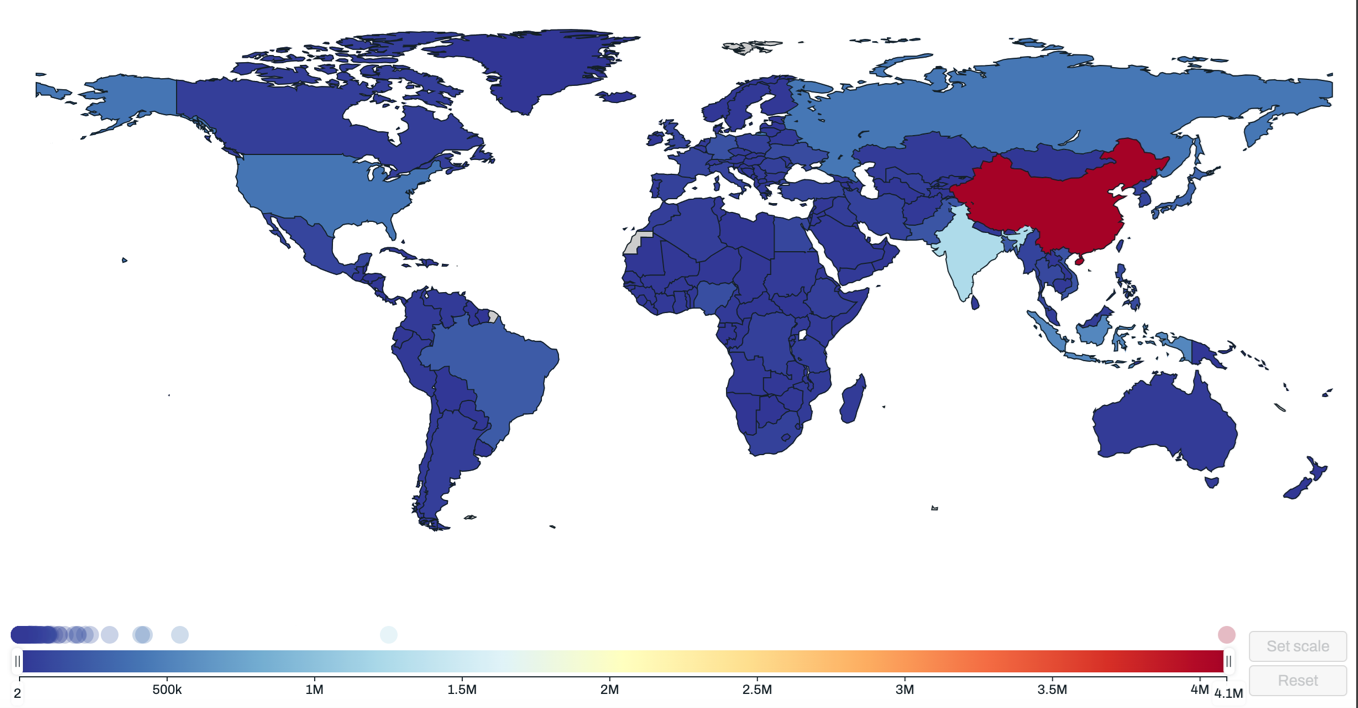
Fig 1. Global stroke burden.
(Source: Institute for Health Metrics and Evaluation (IHME). GBD Compare. Seattle, WA:IHME, University of Washington, 2024.)
China, as one of the world's most populous countries, bears a particularly heavy stroke burden. According to the Brief Report on Stroke Prevention and Treatment in China 2023, a stroke occurs every 10 seconds in China, and every 28 seconds someone dies due to a stroke [2]. The economic burden of stroke in the country is immense, the direct medical costs for stroke treatments, rehabilitation, and productivity losses estimated at RMB 40 billion yuan annually [2].
Similarly, in Hong Kong, stroke remains a leading cause of mortality and morbidity. It is the fourth leading cause of death, with a marked increase in reported cases over the past decade. Surveys conducted by the Census and Statistics Department reveal a 52% increase in reported stroke cases, rising from 37,800 in 2009/10 to 57,500 in 2018/19 [3]. This increase underscores the urgency of addressing stroke prevention, diagnosis, and treatment to mitigate its public health impact.
The Importance of Timely Treatment for Stroke Patients
Strokes are generally classified into two major categories: ischemic stroke, caused by the blockage of an artery in the brain, accounts for over 80% of all strokes; and haemorrhagic stroke, caused by a ruptured brain artery, including intracerebral haemorrhage and subarachnoid haemorrhage, accounts for approximately 20% of all strokes [1]. Without immediate intervention, both types of stroke can result in irreversible damage. Alarmingly, 1.9 million brain cells die every minute from stroke onset. Therefore, timely and accurate treatment is critical to restore blood flow and minimise brain injury. [4] .
For acute ischemic strokes (AIS), timely intervention focuses on dissolving or removing the blood clot obstructing the blood supply to the brain. Major treatment methods include intravenous thrombolysis (IVT), which involves administering thrombolytic drugs intravenously to dissolve the clot blocking blood flow to the brain [5]. For patients who are either ineligible for IVT or when the clot is located in a large artery, endovascular thrombectomy (EVT) can be performed, where a catheter is used to physically remove the clot [5]. These treatments are known as acute reperfusion treatments, which have short time windows. For example, in otherwise eligible cases, IVT has to be administered within 4.5 hours after stroke symptom onset, while EVT has to be conducted within 24 hours after symptom onset [5].
However, multiple factors may prolong the initiation of reperfusion therapy, including transportation, patient transfer, conducting necessary diagnostic tests and examinations, and workflow arrangements, all of which can impact patient outcomes (Fig 2). According to analyses of over 58,000 AIS patients treated with tissue-type plasminogen activator (tPA) within 4.5 hours of symptom onset in the Get With The Guidelines-Stroke Programme (GWTG-Stroke) in the United States, every 15-minute reduction in door-to-needle time (DNT; i.e., interval from arrival to the hospital ("door") to initiating injection of the thrombolytic drug ("needle") ) of IVT increased the likelihood of patients being able to walk independently at discharge by 4%, raised the chance of being discharged home rather than to another facility by 3%, and decreased the probabilities of in-hospital death and serious complications such as symptomatic intracerebral hemorrhage both by 4% [6]. These findings underscore the life-saving importance of streamlining hospital workflows to ensure that stroke treatment begins as quickly as possible.

Fig 2. Workflow factors that may delay the initiation of reperfusion therapy.
For haemorrhagic strokes, rapid treatment is just as vital. The treatment focuses on controlling bleeding and reducing intracranial pressure. Initial treatment often involves medications to lower blood pressure, reverse anticoagulation, or halt bleeding [7,8]. In more severe cases, surgical interventions such as craniotomy or endovascular coiling may be necessary to repair the ruptured blood vessel, drain the blood, and prevent further damage [9]. Early intervention for haemorrhagic stroke can significantly reduce the extent of brain damage and improve the patient’s chances of recovery.
Therefore, rapid and accurate differentiation between ischemic and haemorrhagic strokes is crucial for ensuring appropriate and timely treatment, as the treatments for these two types differ fundamentally. In current acute stroke management workflows, upon arrival to the hospital, patients with a suspected stroke will usually receive physical examinations, necessary blood tests, and brain imaging exams to rule out other conditions that mimic stroke symptoms, such as migraines or seizures, and to differentiate between ischemic and haemorrhagic strokes, enabling appropriate treatment decisions. In current workflows, suspected stroke patients typically undergo a plain computed tomography (CT) brain or 1.5/3.0T magnetic resonance imaging (MRI) brain scans, and in cases of suspected large-vessel occlusion, additional imaging, such as CT or MR angiography, may be required to visualise the blood vessels in the brain.
However, the current workflow for stroke diagnosis is not without challenges. Physical examinations and blood tests are often conducted outside the CT or MRI scan room, requiring patients to be transferred between different locations. Moreover, both CT and MRI scanners need to be operated by radiographers, and the images need to be interpreted by radiologists or neurologists, which places high demands on medical resource coordination and poses a challenge to the efficiency of acute stroke diagnosis and treatment.
Innovative Low-Field MRI Technology
To address these challenges, an innovative imaging technology – low-field magnetic resonance imaging (lfMRI) has emerged as a promising solution for expediting acute stroke diagnosis and triage. In recent years, lfMRI scanners have been gradually applied for acute brain imaging exams, particularly for patients with a suspected stroke or other neurological diseases [10-12]. LfMRI offers several advantages over traditional imaging methods. Compared with CT, it does not use any ionising radiation. Compared with conventional 1.5/3.0T MRI, lfMRI is more cost-effective, requires less space, has no special shielding requirements, and has fewer restrictions related to metal objects. It also operates on standard electrical outlets.
The newly developed 0.23T lfMRI system is particularly well-suited for acute stroke care. It can perform a complete stroke imaging protocol in just 5 to 9 minutes (depending on the scanning sequences). The system is highly accurate in detecting both ischemic and haemorrhagic strokes, as well as ruling out stroke mimics.
A study conducted at the Beijing Tiantan Hospital (BTH) demonstrated that, among 30 patients within 24 hours of system onset, the accuracy of lfMRI in detecting acute haemorrhagic strokes was 100% compared to brain CT, which are considered the gold standard in clinical practice [13]. This was accomplished by a newly developed sequence known as Haematoma Enhanced Inversion Recovery (HEIR), which is specifically designed to detect haemorrhagic lesions [13]. In another study at BTH involving 102 patients with minor ischemic strokes or transient ischemic attacks presenting a few hours to days after symptom onset, the lfMRI demonstrated 96% accuracy in detecting ischemic lesions compared to 3.0T MRI [12].
The advantages of the 0.23T lfMRI system extend beyond its diagnostic capabilities. It is user-friendly and can be operated by trained medical professionals, such as neurologists or nurses, and researchers. Furthermore, the images can be reviewed immediately after scanning on a workstation located in the same room, significantly reducing diagnostic time. Using lfMRI is highly safe, with the only observed complication being claustrophobia, occurring in approximately 1% of cases.
The One-Stop Emergency Stroke Unit Model for Stroke Patient Triage and Treatment
Building on the advancements in lfMRI technology, the Chinese Stroke Association (CSA) initiated a nationwide, multicentre clinical study in 2024, to evaluate a novel approach to acute stroke management. The new one-stop acute stroke management approach, called the Emergency Stroke Unit (ESU), integrates the lfMRI technology into a one-stop framework for stroke diagnosis and treatment. The study aims to evaluate the safety and effectiveness of replacing conventional CT or 1.5/3.0T MRI-based workflows with the ESU model for stroke patient triage and treatment in the acute settings.
Under the new ESU model, suspected acute stroke patients can undergo brain imaging, physical examinations, and necessary blood tests in a single treatment room equipped with an lfMRI scanner. Unlike conventional workflows that require patients to be moved between different areas for imaging, examinations, and blood tests, the ESU consolidates all essential steps into one location. Hence, the model eliminates the need for patient transfers and minimises delays in diagnosis and treatment. Within the ESU, on-site neurologists and stroke nurses can immediately review the imaging results, perform clinical evaluations, and make rapid treatment decisions. For patients diagnosed with ischemic stroke and eligible for reperfusion therapy, the clinical team can immediately proceed to administer IVT within the same treatment room without delay. Alternatively, the patient can be rapidly transferred to an angio-suite for EVT. Similarly, in cases of haemorrhagic stroke, patients can be promptly redirected to appropriate treatment pathways, such as surgery or other interventions.
The ESU model represents a major innovation in stroke care by integrating the entire spectrum of acute care into one physical location. This centralised approach is designed to streamline workflows, eliminate inefficiencies, and ensure that stroke patients receive the fastest possible treatment. Compared to traditional decentralised workflows, where patients are moved between different hospital areas, the ESU significantly reduces the time to diagnosis and treatment. By expediting care, the ESU model has the potential to improve outcomes for stroke patients. (Fig 3).
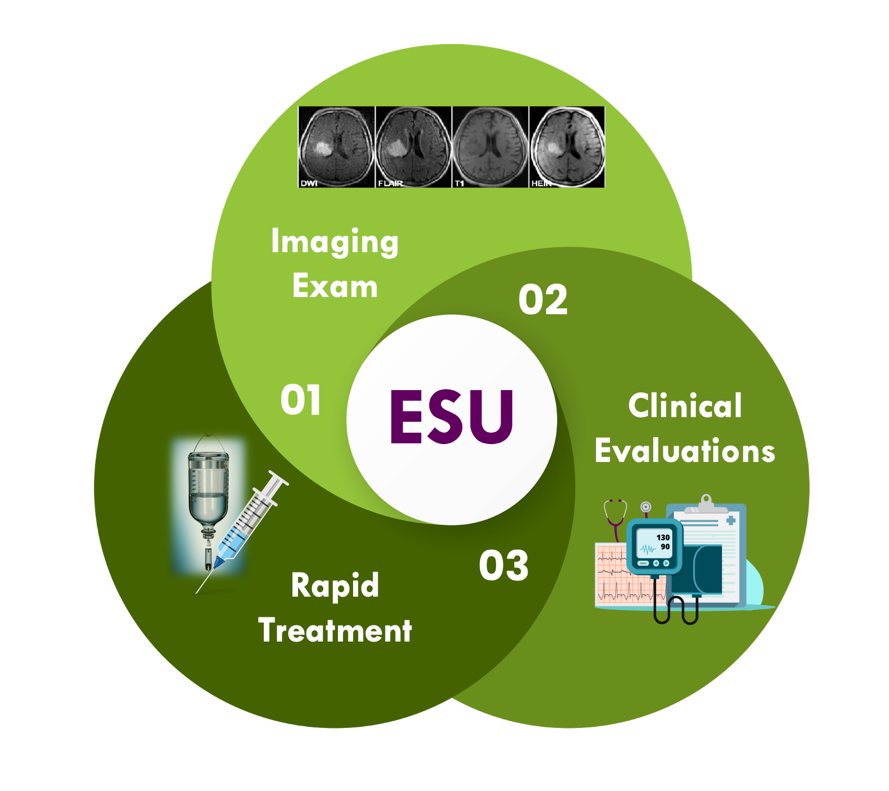
Fig 3. The "One-Stop" Emergency Stroke Unit (ESU) Model
As part of the national multicentreclinical study, the first pilot site for this innovative model in Hong Kong has been established at CUHK and PWH. In August 2024, the 0.23T lfMRI system was installed in the Accident and Emergency Department at PWH to support the implementation of the ESU model (Fig 4). In collaboration with CSA and BTH, the clinical and research team at CUHK and PWH will further validate the safety and accuracy of the lfMRI in diagnosing acute ischemic and haemorrhagic strokes in more than 4,000 patients across China in this study.
Locally, CUHK and PWH are also conducting a dedicated study to assess the impact of the ESU workflow on improving treatment efficiency for AIS patients. Specifically, the study will evaluate the safety and efficacy of the ESU workflow in shortening the door-to-needle or door-to-groin puncture time for AIS patients receiving IVT or EVT. By comparing the ESU model to conventional workflows that rely on CT or 1.5/3.0T MRI, the study aims to explore the feasibility of the ESU model in improving treatment efficiency, optimising medical resource allocation, and enhancing the overall quality of patient care. The research team hopes the findings of the clinical study will not only advance stroke research but also facilitate the clinical application of the ESU model in Hong Kong.

Fig 4. The ESU at the Accident and Emergency Department at PWH.
A. Overall layout of the ESU room.
B. Neurologist and stroke nurse conducting a lfMRI exam.
C. Stroke nurse preparing for IVT in the ESU.
Stroke prevention and stroke symptom recognition
Stroke is a life-altering event with profound impact for patients, their families, and society. Statistics reveal the immense burden of stroke: over two-thirds of stroke survivors require rehabilitation after discharge, 35-40% experience limitations in performing daily living activities within six months after a stroke, 40% suffer from moderate to severe disabilities, and 10% require long-term care in specialised facilities [14]. Beyond the physical and emotional toll, the societal costs of stroke, including healthcare expenses and lost productivity, are staggering. Thus, it underscores the urgent need for widespread public awareness about stroke prevention, early recognition of symptoms, and swift action during emergencies.
Stroke prevention begins with proactive steps in daily life. The leading risk factors for stroke include high blood pressure, diabetes, high cholesterol, smoking, obesity, physical inactivity, and excessive alcohol consumption, etc [1]. Additionally, certain medical conditions such as atrial fibrillation and other heart diseases, also significantly increase stroke risk. Proactively monitoring and controlling these risk factors through a combination of medications, lifestyle interventions, and regular medical follow-up is vital for prevention. Studies show that up to 80% of strokes are preventable through healthy lifestyles and early management of risk factors [8,15]. Key prevention strategies include:
- Get regular check-ups for "triple H" conditions (high blood pressure, high blood glucose and high lipid levels)
- Quit smoking
- Reduce excessive alcohol consumption
- Maintain a healthy weight with a Body Mass Index (BMI) lower than 25
- Keeping a balanced diet consisting of mainly vegetables and some meat, and actively decrease fat, salt and sugar intake
- Exercise regularly (defined exercising at least 150 minutes of moderate-intensity aerobic physical activity, such as brisk walking or hiking, weekly)
However, when a stroke occurs, recognising the symptoms quickly and seeking immediate medical attention are equally important. The sooner the person takes heed of the symptoms and receives treatment for a stroke, the less damage is likely to happen. Remember the warning signs of stroke (Fig 5), and act fast for help if you suspect that you or your family member is having a stroke. The warning signs of a stroke include:
- F: Face Drooping – Has their face fallen on one side? Can they smile?
- A: Arm Weakness – Can they raise both arms and keep them there?
- S: Speech Difficulty – Is their speech slurred?
- T: Time to call emergency medical help (e.g., 999 in Hong Kong) if you see any single one of these signs
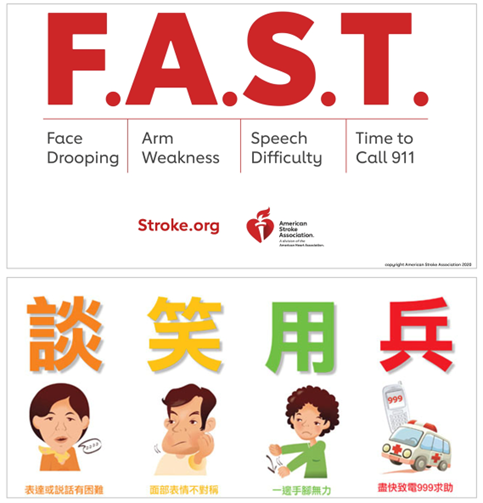
Fig 5. "FAST" (upper panel) for stroke symptom recognition and immediate action to call emergency services, and "談笑用兵"- the Hong Kong version of FAST (lower panel).
(from https://newsroom.heart.org/file?fid=57115a9a2cfac21d8f71e4f0 and https://www.strokefund.org/prevention_part1.php)
Other possible stroke symptoms like sudden onset of numbness, vision problems, dizziness, sudden severe headache, confusion, or loss of balance should also prompt urgent medical evaluation, as "time is brain."
The more rapidly a stroke victim receives treatment to restore blood flow, the higher the chances of survival with good neurological outcomes.
Conclusion
The introduction of lfMRI technology and the ESU model marks a significant breakthrough in stroke care in Hong Kong. This comprehensive one-stop approach for acute stroke triage and treatment represents a paradigm shift that could substantially improve outcomes on a global scale. The initiation of this major multicentre clinical study will generate invaluable real-world evidence on the accuracy, safety, and potential benefits of integrating lfMRI into hyperacute stroke protocols. The findings have the potential to transform best-practice standards for healthcare systems worldwide in the quest to optimise acute stroke management.
In parallel with these vital advances in acute stroke care, CU Medicine and PWH will continue prioritising public education around primary stroke prevention through risk factor modification and the adoption of a healthy lifestyle. Empowering the community with the knowledge to reduce their stroke risk and recognise warning signs swiftly is equally crucial to combat stroke and its devastating effects. The team will also continue to drive relevant research and explore new technologies to enhance the efficiency and outcomes of stroke care, benefiting patients locally and globally.
References:
- Feigin VL, Brainin M, Norrving B, Martins S, Sacco RL, Hacke W, et al. World Stroke Organization (WSO): Global Stroke Fact Sheet 2022. Int J Stroke. 2022;17:18-29.
- 《中國腦卒中防治報告2021》概要. 中國腦血管病雜誌. 2023;20:783-793.
- Non-communicable Disease Branch, Centre for Health Protection of the Department of Health: Stroke Awareness and Prevention. https://www.chp.gov.hk/files/pdf/ncd_watch_october_2021.pdf, 2021.
- Saver JL. Time is brain—quantified. Stroke. 2006;37:263-266.
- Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50:e344-e418.
- Saver J, Fonarow G, Smith E, Reeves M, Grau-Sepulveda M, Pan W. Time to treatment with intravenous tissue plasminogen activator and outcome from acute ischemic stroke. JAMA. 2013;309
- Brouwers HB, Goldstein JN. Therapeutic strategies in acute intracerebral hemorrhage. Neurotherapeutics. 2012;9:87-98.
- Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-Hill D, et al. 2021 Guideline for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline From the American Heart Association/American Stroke Association. Stroke. 2021;52:e364-e467.
- Mayo Clinic: Intracranial hematoma - diagnosis and treatment. https://www.mayoclinic.org/diseases-conditions/intracranial-hematoma/diagnosis-treatment/drc-20356149.
- Yuen MM, Prabhat AM, Mazurek MH, Chavva IR, Crawford A, Cahn BA, et al. Portable, low-field magnetic resonance imaging enables highly accessible and dynamic bedside evaluation of ischemic stroke. Sci Adv. 2022;8:eabm3952.
- Mazurek MH, Cahn BA, Yuen MM, Prabhat AM, Chavva IR, Shah JT, et al. Portable, bedside, low-field magnetic resonance imaging for evaluation of intracerebral hemorrhage. Nat Commun. 2021;12:5119.
- Suo Y, Xie X, Zhang Z, Gong X, Xu Y, Wei N, et al. Mobile 0.23 T MRI detects cerebral infarction in patients with minor ischemic stroke or TIA. Stroke. 2024;5:e249–e251.
- Xie X, Jiang Q, Suo Y, Han C, Wang Z, Zhang Z, et al. 0.23-Tesla MRI to differentiate between ischaemic and haemorrhagic strokes within 24 hours of onset: a combined experimental clinical study. Stroke and Vascular Neurology. 2024;ahead of print:svn-2024-003592.
- American Stroke Association: Stroke Rehabilitation. https://www.stroke.org/en/life-after-stroke/stroke-rehab
- Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet Neurology. 2021;20:795-820.
- American Stroke Association: Stroke symptoms. https://www.stroke.org/en/about-stroke/stroke-symptoms
- Strokefund: 急救中風 - 談笑用兵. https://www.strokefund.org/prevention_part1.php
Authors:
Prof Xinyi Leng, Assistant Professor, Department of Medicine and Therapeutics, The Chinese University of Hong Kong
Prof Thomas W Leung, Lee Quo Wei Professor of Neurology and Head of the Division of Neurology in CU Medicine's Department of Medicine and Therapeutics; Director and Honorary Consultant of the Acute Stroke Unit, Prince of Wales Hospital
December 2024